Lisa Frain
Sep 27 2023
Reading Time: 3 minutes
Industry-wide staffing shortages and ongoing regulation changes continue to put pressure on post-acute providers. Dated documentation methods only add to the problem, putting even more administrative burden on clinicians who struggle to update patient records between visits and after hours. With technology that allows staff to document at the point of care, staff gain more work-life balance and patients gain a better care experience.
Despite a clear need for a documenting solution, many organizations continue to use dated methods of capturing data.
Let’s look at five consequences of not documenting at the point of care:
1. It can give staff poor work-life balance.
It’s not uncommon for clinicians to struggle completing their documentation during the workday, forcing them to take their work home to finish after hours — ultimately keeping them from spending time with their families. This delay in documentation can also leave the clinicians with questions, requiring additional follow-ups with the patient. The result is more work and more stress.
Documenting at the point of care relieves the stress of working in the evenings and increases staff satisfaction.
2. It can cause documentation inaccuracies and lower quality of care.
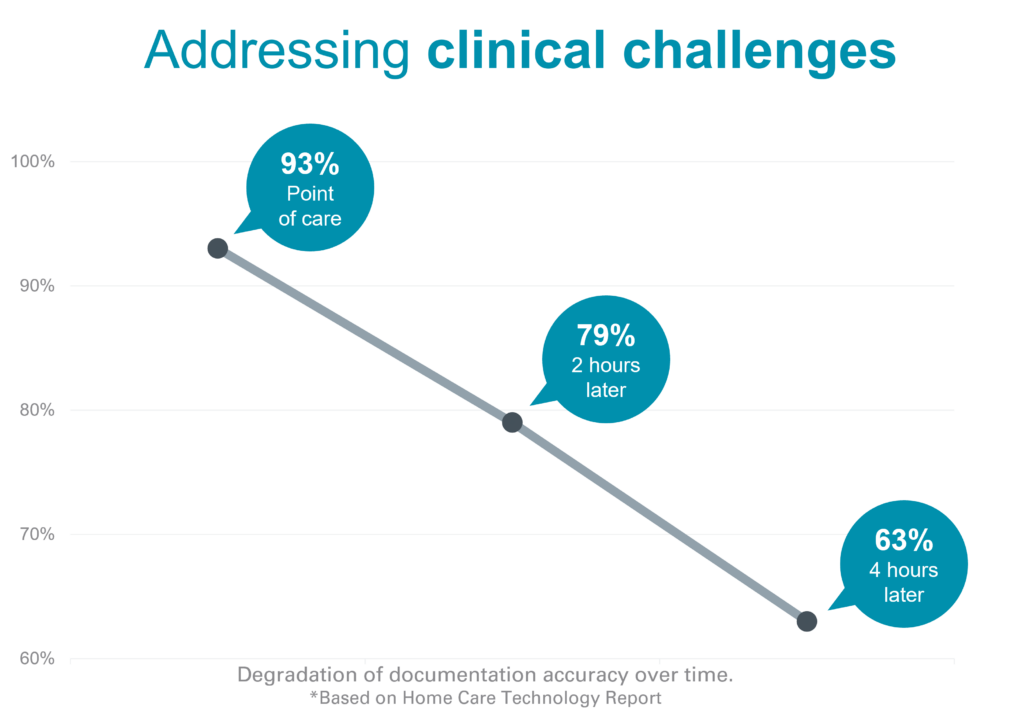
Clinicians often must write notes by hand during visits to later enter the data manually into the EHR, which can cause inaccuracies due to human error. According to the Homecare Technology Report, clinicians have been shown to only document at 63% accuracy when the documentation is completed four hours following the visit.
In addition to the inaccuracies they can cause, handwritten notes are unsecure, can be misplaced or can be seen by someone outside of the care team.
Point-of-care documentation offers real-time collaboration, a proactive approach that decreases the risk for error and gives staff more time with patients.
3. It can create safety concerns.
When documentation is done manually, patient data can’t be used to help clinicians make more informed decisions. With point-of-care documentation, alerts can be addressed in real time — such as medication reconciliation triggering a problem that needs immediate attention.
Continued education with the patient and caregiver is also promoted when documenting at the bedside, empowering patients to take part in their care journey.
4. It can reduce productivity.
Documenting at the point of care allows staff to streamline the important work they do and complete more visits in a day. It allows clinicians to do more with less, while increasing engagement and job satisfaction.
5. It can negatively impact billing and reimbursement.
Billing or claim rejections will happen now and then, but the right digital tools will maximize your cash flow. This is due to better accuracy and efficiency happening at the point of care, ultimately increasing timely reimbursement.
Ready to experience what point-of-care documentation can do for your organization? Talk to a CitusHealth expert to learn about the digital tools we have to offer.