Ivana Andrews
Oct 19 2023
Ivana Andrews
Oct 19 2023
Reading Time: 6 minutes
As reimbursement changes and rate cuts keep coming for our industry, there’s no doubt that staying profitable and competitive is a top priority for every home-based care provider. So how do you make sure to hit the mark at your organization?
Think about it. By emphasizing patient care throughout the entire continuum of care, providers can deliver cost-effective, high-quality care in the right place at the right time. As a result, the likelihood of medication errors, adverse events and re-hospitalization drops significantly – and these better patient outcomes translate into better performance on quality measures that influence everything from reimbursement to referrals.
In fact, providers who implement a solid patient care strategy can benefit from a reduction in penalties under home health value-based purchasing as well as higher patient satisfaction for improved HHCAHPS scores. And when nurses and other caregivers on your home healthcare team feel supported in their goal of providing better patient care, they become more satisfied, leading to better retention rates for your business.
Here are 4 must-haves to help your organization focus on improving the quality of care you deliver to your patients.
1. Communicate in patient’s preferred method in real time.
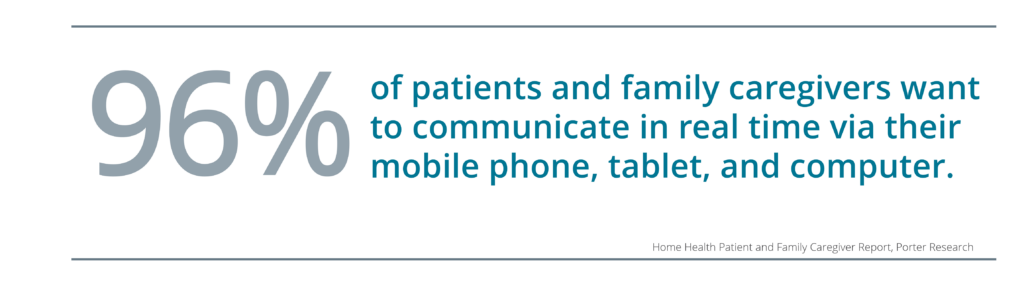
This statistic from consumer research we conducted says it all: 96% of your patients and family caregivers want to communicate with you in real time using their mobile phone, tablet or computer. You can answer this call by developing an omni-channel communication strategy that delivers on what today’s tech savvy consumers expect from their home healthcare providers.
This digital consumer experience allows patients to manage prescriptions, book appointments, complete paperwork, get reminders and even connect directly to on-call nurses and other clinicians for added support with questions like, “Hey, when’s my visit tomorrow?” Or “I need help to understand what this medication is.” And it’s not just about engaging patients in these modes they prefer. You’ll also want to do so in their preferred language through integrated automated translation services.
How does this relate to reimbursements and referrals? Meeting your patient’s expectations with a digital experience gets reflected in HHCAHPS survey scores and relayed back to referral sources.
2. Provide patient and family caregiver education on demand.
We can’t educate our homecare patients enough. There’s a lot of information being thrown at them, and it’s a difficult time in their lives. Plus, they may be working with your organization as well as an HME and home infusion provider, with packets of instructions from everyone. One stat that always sticks with me is that less than 60% of patients can even remember the diagnoses addressed during their inpatient stay.

By ensuring your training resources are therapy specific, electronic, and on demand 24/7 from anywhere, anytime and any device, you empower patients and family caregivers to have the education they need and the peace of mind that the information you’ve provided is always accurate and up to date.
Your patients can confidently answer that you offered education on their care plan during the HHCAHPS survey, and the improved patient experience can significantly impact outcomes because good education equals lower chances of ER visits or re-hospitalization.
3. Embrace telehealth.
Being able to use digital tools to connect and provide support to patients remotely is a huge win for patient care and has become a common expectation among patients and family caregivers ever since the pandemic. Photos and videos can be used to check in on patients in between home visits, to quickly troubleshoot questions related to medications and equipment, and to assess complex wound care faster.
And that last point about telehealth helping to address wound care is especially important since we know that over 8 million patients suffer from wounds in the US annually, and certified wound nurses are in short supply.
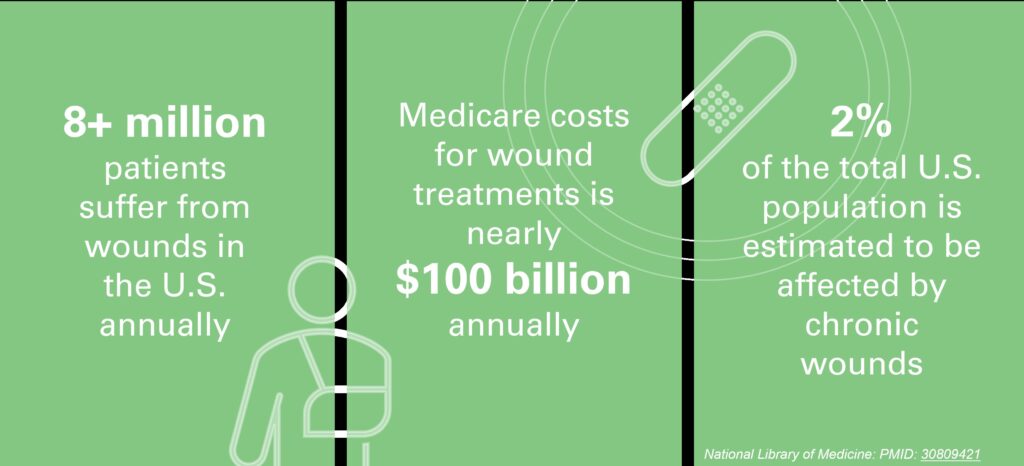 When you can hop on a video chat to make sure a patient is staying compliant with their medication regiments and to assess the condition of wounds and swelling, you’re improving patient care. You’re also helping to scale despite a nursing shortage. Instead of having to turn away referrals, telehealth allows one nurse to take care of more patients to drive up your census and help with rate cuts.
When you can hop on a video chat to make sure a patient is staying compliant with their medication regiments and to assess the condition of wounds and swelling, you’re improving patient care. You’re also helping to scale despite a nursing shortage. Instead of having to turn away referrals, telehealth allows one nurse to take care of more patients to drive up your census and help with rate cuts.
4. Reduce hospitalizations.
We know that more than 7 million patients are impacted by preventable medical errors every year to the tune of $21 billion across all care settings. And 16% of unplanned readmissions within 30 days are medication related, so it’s of utmost importance to think about ways to decrease these incidents.
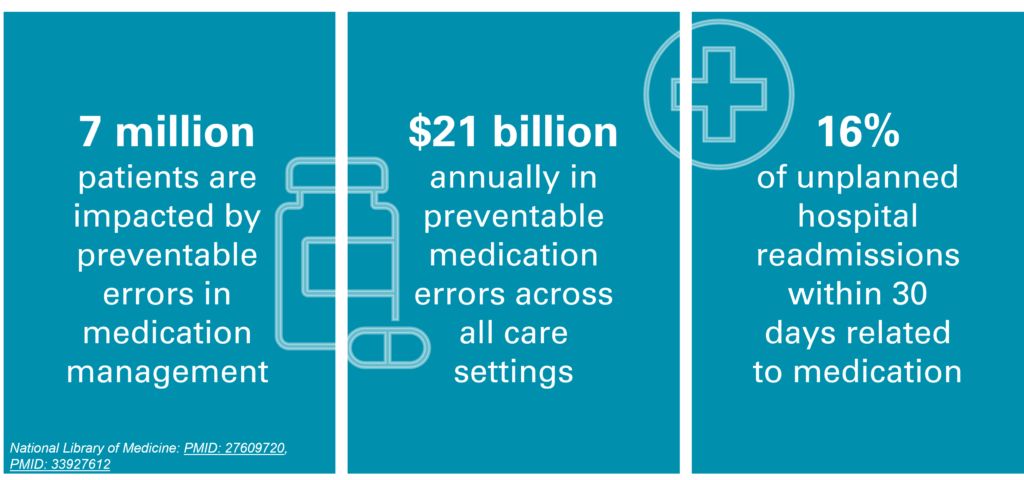
Digital technology is, without a doubt, an excellent way to drive early interventions that reduce re-hospitalizations because it lets you keep a beat on what’s going on in between visits. Let’s say you have a CHF patient with increased swelling in their ankles or feet. With virtual medication management, home-based care providers can change medications without the need to see the patient in person, using customized digital forms to electronically send refill or change requests, get them promptly filled and avoid delay of care for the patient.
Digital technology can keep nurses and other caregivers ahead of adverse events that might be coming around the corner, prompting them to intervene before it becomes an event that leads to re-hospitalization.
We all want our patients to do well under our care; but, in home-based care, you’re not there all the time. Digital approaches can make it feel like you are. You won’t have to skip a beat in providing the highest level of patient care by communicating more efficiently in the patient’s preferred digital method, providing excellent education so they don’t have to search elsewhere, and embracing telehealth and reducing re-hospitalization for improved outcomes. Put these must-have measures in place and then don’t be surprised to see higher satisfaction scores on surveys, a larger patient census and increased referrals and reimbursements.
Ready to see how technology can take your organization to the next level? Schedule a demo to see for yourself.