Melissa Kozak
May 12 2023
Melissa Kozak
May 12 2023
Reading Time: 3 minutes
Care teams need a holistic view of the patient in real time, which is why interoperability has become such a necessity in home-based care. In fact, it’s an expectation for organizations to use digital tools that allow for the secure and efficient exchange of patient information.
Point solutions for remote care can make interoperability more challenging and create too much work for health system IT teams to tie everything together. These solutions disrupt the care-at-home promise of a holistic view of patient health, which is why end-to-end solutions are key.
The cost of non-interoperable solutions, including duplicative workflows and increased administrative work, is too high — negatively impacting effective care and the bottom line — indicating a clear need for technology built to support interoperability.
Needing early interventions
With the shift to value-based care, reducing readmissions is imperative. Connected and collaborative care means data can follow the patient and be acted upon in real time. With technology that supports interoperability, costly preventable readmissions can be avoided.
Embracing true interoperability
According to HIMSS, interoperability is the ability of different information technology systems and software applications to communicate, exchange data and use the information that has been exchanged. It’s not just about technical specifications, but also requires the engagement of multiple stakeholders and the use of workflows.
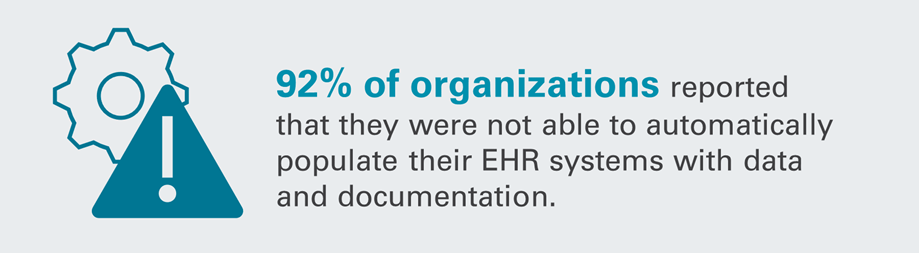
92% of organizations reported that they were not able to automatically populate their EHR systems with data and documentation.
Top frustrations among referring providers with post-acute organizations that do not accept electronic referrals include playing phone tag, the inability to see how patients are progressing, the inability to accept all payors, and meeting timeframes for performing initial service.
With true interoperability, the data flows between the referring provider’s EHR system and a patient record on the post-acute care provider’s system. This eliminates the need for duplicate data entry and creates less risk of human error or lost orders, ultimately resulting in higher staff efficiencies.
Connecting with nationwide data exchange
Organizations dedicated to driving health data exchange like CommonWell Health Alliance and Carequality are helping to improve coordinated care and health outcomes by securely and efficiently connecting home-based care providers and referral partners. CitusHealth integrates with these data exchange organizations to keep our users connected, helping to ensure smooth transitions of care and up-to-date patient information.
CommonWell Health Alliance connects more than 30,000 providers, 180 million unique individuals and 3 billion health records. Carequality connects 600,000 providers, 50,000 clinics and more than 4,200 hospitals.