Melissa Kozak
Dec 7 2022
Reading Time: 4 minutes
By: Melissa Kozak, RN, BSN, President & Co-Founder, CitusHealth
Since its implementation in 2016, the Home Health Value-Based Purchasing (HHVBP) Model has been a success, resulting on average in a 4.6% improvement in HHA performance and an annual savings to Medicare of about $141 million. These results led to the expansion of the original HHVBP Model to continue to reduce Medicare spending and improve quality of care.
On January 8, 2021, CMS announced its intent for this nationwide expansion, with 2022 established as the pre-implementation year for agencies to set the bar for performance. 2023 will be the performance year, which will be measured against 2022’s baseline. In 2025, the first payment year, revenue adjustment amounts will be upward or downward of 5%, which will be determined on CY 2023 VBP performance scores.
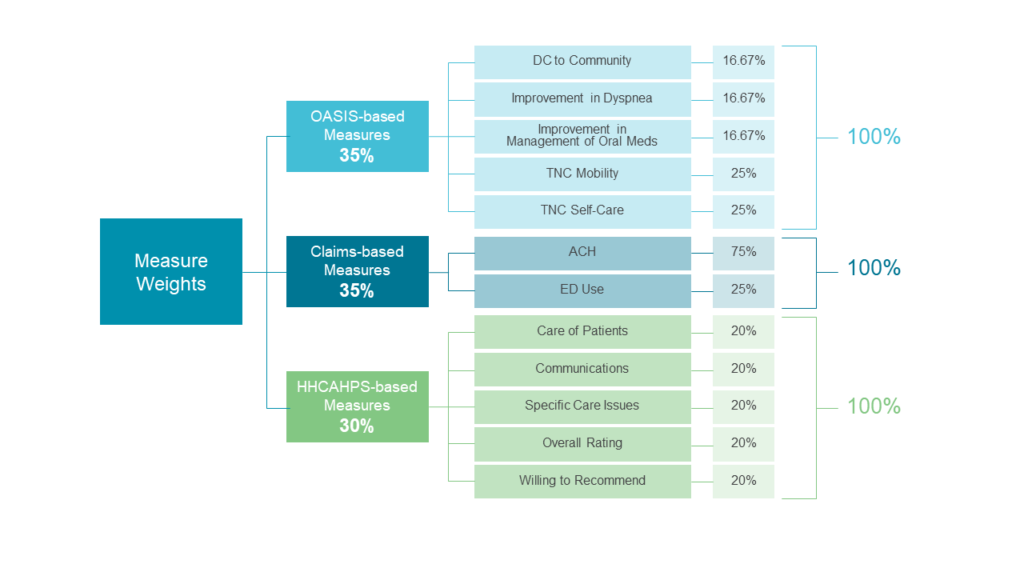
These Total Performance Scores are weighted into three categories: HHCAHPS scores, claims-based data, and OASIS-based data. Here, we’ll discuss these measures and why they’re top drivers of HHVBP reimbursement rates.
How HHCAHPS scores drive reimbursement rates in home-based care
The Consumer Assessment of Healthcare Providers and Systems Home Health Care Survey (HHCAHPS) is designed to measure the experiences of people receiving home health care from Medicare-certified agencies. There are five HHCAHPS survey-based measures:
The CitusHealth Message Center can help meet HHCAHPS goals
Meeting these survey expectations all comes down to communication. With the right digital tools, HHAs get secure, real-time communication on any device — driving patient and caregiver satisfaction, improved HHCAHPS scores, and ultimately better Total Performance Scores.
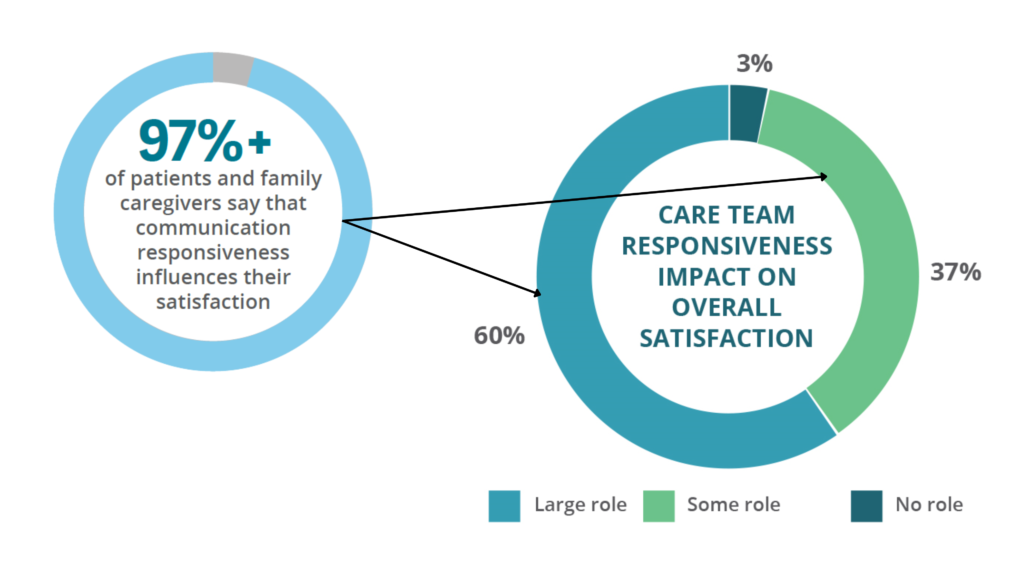
Source: Porter Research Survey
How claims-based measures drive reimbursement rates
Medicare fee-for-service claims data provides insight into the rehospitalization of home health patients, which can lead to revenue adjustments. There are two claims-based measures:
Meeting these claims-based expectations means recognizing adverse events before they lead to unnecessary rehospitalizations. Poor medication management and safety in the home are top reasons for rehospitalization, but the good news is that HHAs can use technology in a number of ways to help patients better adhere to their medications and receive care safely in the home.
The CitusHealth Education Center and Message Center can help meet claims goals
Digital education empowers patients to take ownership in their care and eliminates the need to rely on stacks of paper education materials that are likely to get misplaced. It also helps to educate patients on safe home environments — such as how to use crutches correctly or using handrails in the bathroom. Video chat capabilities allow the nurse to reinforce safety measures or look at a shoebox full of medication to help patients understand what to take and when. More streamlined, real-time communication channels with the nurse help to educate on signs and symptoms of side effects, etc.
Other drivers for rehospitalizations are language and literacy barriers. With automatic language translation built into the message center, this barrier is removed between nurses and patients, allowing them to openly communicate in their native languages.
How OASIS drives reimbursement rates in home-based care
Outcome and Assessment Information Set (OASIS) is a standardized data set that measures quality and outcomes. There are five measures for HHVBP:
OASIS measurements largely rely on clinical documentation that captures daily activity and mobility data. Poor results are due to lack of improvement, which can lead to HHVBP payment adjustments.
The CitusHealth Forms Center can help meet OASIS goals
With the right technology, check-in forms can be customized and electronically sent to patients, allowing them to respond on their own time and on a device of their choosing. This check-in approach keeps staff updated on patient status, reminds patients to execute plans of care, and reinforces ongoing education on their care.
As we all know, improving your connection with patients will help with preparing for the HHVBP Model and your software platform will play a critical role in your success. Don’t be behind when the CY 2023 performance year begins.
Schedule a CitusHealth demo today to learn more about how we can help your agency meet HHCAHPS, claims, and OASIS goals — and how that will help you succeed in the coming HHVBP performance year.